The Biochemical Reality of B6 Toxicity, Neuropathy, and Functional Overload
A quick note:
I’ve held off on writing this for a while—not because the data wasn’t there, but because the public dialogue around B6 toxicity has been so profoundly lacking.
What’s being published is vague, mechanistically empty, and often flagrantly wrong.
I’ve seen B6 toxicity dismissed outright, blatantly misunderstood, or treated in ways that legitimately make things worse.
I’ve dealt with it personally, and I’ve seen patients go through it. And I can’t ignore how absurdly inadequate the available information is. Most people commenting on B6 toxicity simply don’t know what they’re talking about.
I don’t think there’s any other article out there—at least at the time of this writing—that lays out the actual mechanisms and theory behind B6 toxicity this clearly, especially for a non-technical audience.
Mind you—this isn’t everything. But this’ll give you a better idea of what you’re dealing with.
If you know anyone dealing with this, please share this article. They may not find anything better.
I hope this helps.
~ Dr. Malek
What Makes Vitamin B6 Dangerous for Some People?
What Is Vitamin B6 and Why Is It Prescribed So Often?
Vitamin B6 is extremely widely used—It’s commonly recommended for symptoms and diseases as broadly arrayed as:
Morning sickness and nausea in pregnancy
PMS and mood swings
Fatigue and adrenal dysfunction
Carpal tunnel syndrome
Peripheral neuropathy
Depression and anxiety
Histamine intolerance
High homocysteine and methylation support
Insomnia and low serotonin
Cognitive decline and Alzheimer’s risk
Immune regulation and inflammation
Detoxification and sulfur metabolism
Hormonal imbalance and estrogen clearance
It’s found in most multivitamins, nearly every B-complex, and an increasing number of energy drinks, protein powders, hydration powders, and “methylation support” supplements. Many people take B6 daily, often in doses in the hundreds of milligrams per day.
And it can occur even without supplementation. Read about that in my article (it’s the only of its kind currently available on the web).
Yet, for an important subset of individuals, vitamin B6 can cause an array of truly debilitating toxicity symptoms—including tingling, anxiety, and insomnia—even when their blood levels of B6 appear normal or high.
Even if it’s improving your morning sickness, insomnia, or depression, it can simultaneously be causing—quite casually—a true biochemical derangement of its own: One that’s genuinely very difficult to get out of without incredible precision or—in the absence of precision—patience.
This goal of this article is to explain exactly what’s happening.
B6 Reactions are Surprisingly Common and Often Dismissed
Early Symptoms of Vitamin B6 Toxicity that Most Miss - Overstimulation, Anxiety, and Sleep Disruption as Red Flags
B6 toxicity most commonly impacts the peripheral nerves first—at least that’s where noticeable symptoms tend to first crop up.
You’ll feel things like:
Tingling, burning, buzzing, electric shocks in feet or hands
Mental catastrophizing
Sudden insomnia or feeling “wired but tired”
Panic episodes, facial tension, sensory overstimulation
Brain fog, clumsiness, imbalance
Feeling worse on multivitamins or B-complex supplements
These early signs are sometimes misdiagnosed, but they are well-documented features of pyridoxine neuropathy—a common form of vitamin B6-induced nerve dysfunction.
Many people miss these early signs of B6 toxicity or mistake them for unrelated side effects.
How B6 Toxicity Damages Your Nerves
Neuropathy and the Role of the Dorsal Root Ganglia
An essential element is peripheral neuropathy, like the kind that develops with diabetes: tingling/burning in the toes or fingers, though the toes are usually first.
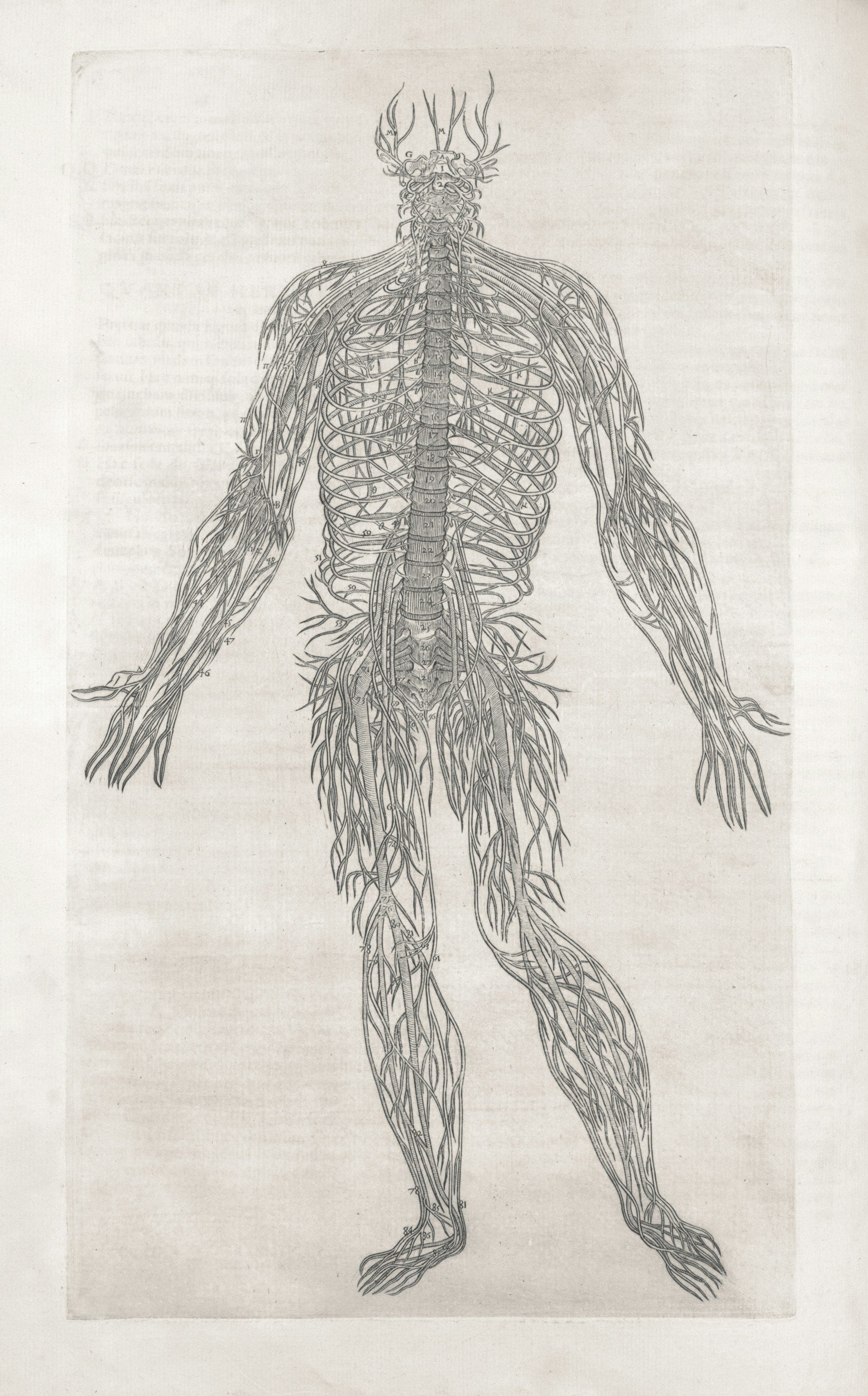
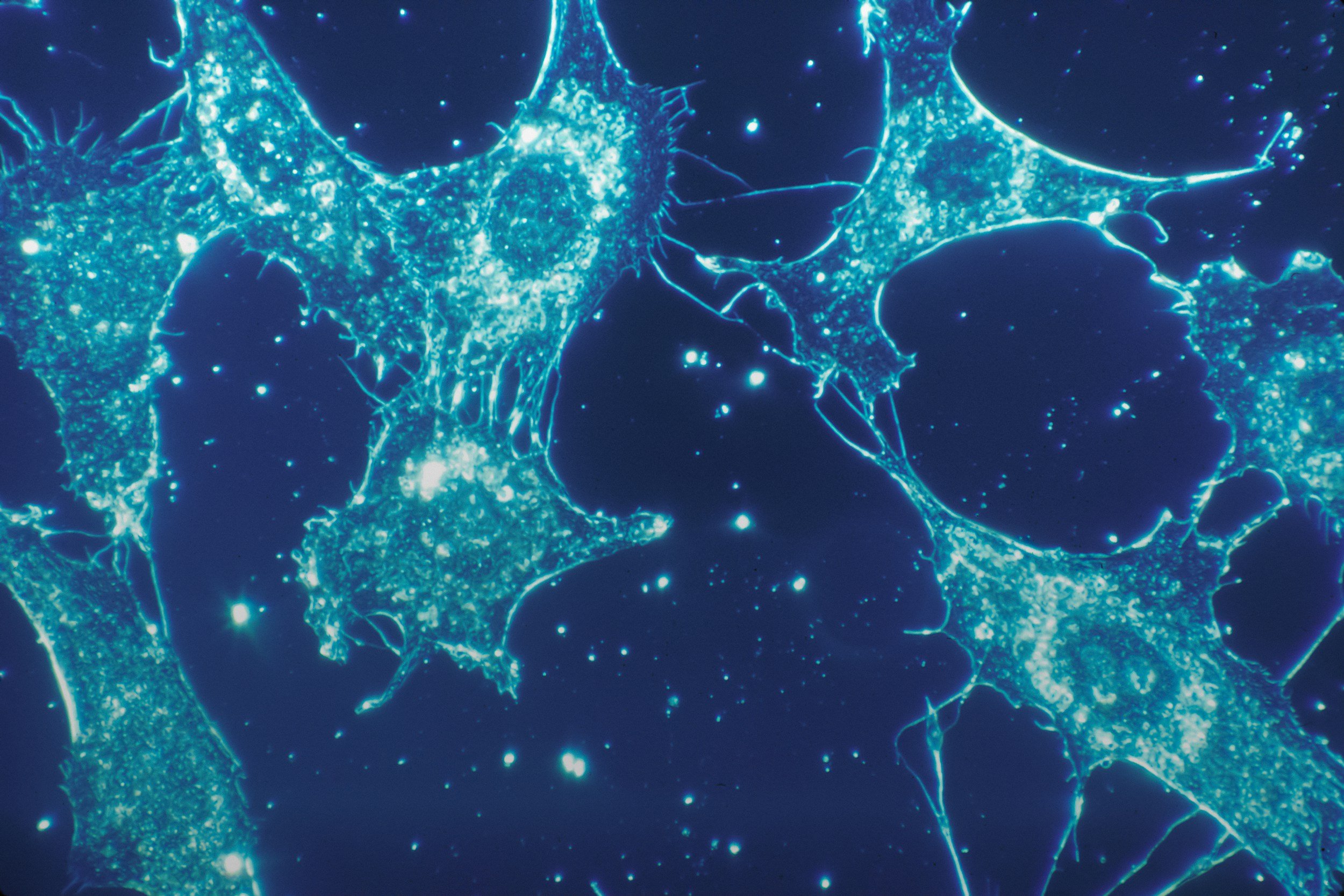
The reason your toes and fingertips are first affected is tied to specific nerve clusters called the dorsal root ganglia (DRG).
The DRG are bundles of sensory nerve cell bodies located just outside your spinal cord. Their primary job is to relay sensory signals—things like pain, vibration, touch, temperature, and proprioception—from your extremities (especially your toes and fingers) up to your brain.
But these ganglia are uniquely vulnerable:
They have a relatively weak protective barrier, making them more exposed to toxins like excess B6.
They're highly metabolically active, meaning they depend heavily on energy production (mitochondrial health).
Their long nerve fibers extend to your feet and hands, requiring constant maintenance and perfect functioning.
This pattern is classic for sensory neuropathy from B6, and often described as a “stocking-glove” distribution.
Less Obvious Signs of B6-Induced Neuropathy
When vitamin B6 accumulates in these delicate sensory neurons, it disrupts their internal metabolism and energy production, ultimately causing nerve damage. This is why the earliest signs of true B6 toxicity often show up as tingling, burning, and sensory changes in the farthest points from the DRG: your toes and fingertips.
Such damage will be:
Primarily sensory: affecting sensation first, sparing strength or movement initially
Symmetrical and "stocking-glove" distribution: starting equally on both sides, in distal extremities (feet/hands)
Slowly progressing upward: toes → feet → ankles, then handsAssociated with loss of vibration or proprioception (difficulty sensing joint position or balance, especially noticeable in the dark)
Occasionally accompanied by subtle autonomic or mood-related symptoms (anxiety, irritability, hypersensitivity), though these tend to be secondary to sensory nerve dysfunction
People often become toxic after the recommendation of a healthcare practitioner.
Doctors and general healthcare professionals alike are taught to generally consider all B vitamins as “water-soluble and safe” and thus impossible to overdose on.
This is entirely incorrect. Regardless of water solubility, every exogenous substance that enters your body has certain mechanisms by which the body gets rids of its. The particular configuration of those mechanisms determines that substance’s half-life—a statistical measure that gives you an idea of how quickly it’s gotten rid of.
The half-life of B6 is a matter of several weeks, meaning that it takes months to truly eliminate—depending on how high your levels went.
Why B6 Toxicity Is Not Just About Dose
Most discussions of vitamin B6 toxicity begin and end with dosage. Conventional sources cite cases of neuropathy linked to doses exceeding 500 mg/day, or chronic use over 1,000 mg/day. While that is technically true, it's also highly misleading.
Low Dose B6 Toxicity—Why Even 25–50 mg (or less) Can Trigger Overdose Symptoms
In clinical practice—and in published case reports—symptoms of B6-induced nerve damage have been observed at doses as low as 50 mg/day, sometimes even lower, particularly when taken over extended periods. In a 1987 case series, sensory neuropathy symptoms were found in patients taking as little as 50 mg/day of pyridoxine (Dalton, K., & Dalton, M. J. T. (1987).
Some individuals experience symptom onset within weeks, while others tolerate high doses for years before any obvious signs appear.
B6 Toxicity Is a Biochemical Mismatch, Not Just Overdose
This variability isn't random.
It reflects something crucial: B6 toxicity is not a fixed threshold. It’s a dynamic interaction between dosage, duration, enzyme activity, cofactor status, and genetic vulnerability.
A person’s capacity to metabolize, distribute, and clear B6 depends on a series of tightly regulated intracellular systems. If any of those systems are partially impaired—due to genetics, nutrient deficiency, toxicant exposure, or inflammation—then the individual may begin accumulating B6 (or suffering from its effects) at otherwise “normal” intakes.
In other words: toxicity doesn't require abuse. It only requires a mismatch between input and handling capacity.
How B6 Causes Neurological Dysfunction
Pyridoxine toxicity is not limited to overdose. Even moderate doses can impair vitamin B6 metabolism through PLP enzyme inhibition and downstream overload.
There is no single mechanism of injury behind B6 toxicity. Instead, there are several converging pathways through which B6—especially in supplemental form—can impair nerve health.
The 4 Main Biochemical Mechanisms Behind B6 Toxicity
These include:
• Pyridoxine Interference at B6-Dependent Enzymes
Pyridoxine, the synthetic form used in most supplements, can accumulate in tissues and interfere with the function of enzymes that require the active coenzyme form, pyridoxal-5'-phosphate (PLP). This antagonistic effect has been observed in dorsal root ganglion neurons in multiple animal studies and is believed to underlie some of the sensory-specific neuropathy seen in humans.
• Overactivation of B6-Driven Pathways
B6’s role is to facilitate reactions—it’s a coenzyme in over 140 enzymatic processes. But too much coenzyme activity in a system with bottlenecks leads to biochemical instability. This can include:
Overproduction of excitatory neurotransmitters (e.g., glutamate)
Overactivation of transsulfuration (leading to cystathionine or sulfite accumulation)
Depletion of intermediary substrates (e.g., glycine, taurine, glutamine)
Rather than blocking enzymes, in some people B6 accelerates them into dysfunction.
• Nutrient Cofactor Exhaustion
B6-dependent enzymes also depend on other nutrients: magnesium, riboflavin (B2), zinc, iron, etc.
When B6 levels rise, these cofactors can become limiting. The result is a partial or complete stall-out of dependent reactions, with collateral accumulation of metabolic intermediates.
• Genetic and Epigenetic Variant Weak Points in B6 Regulation
Genetic variants in enzymes such as PDXK (pyridoxal kinase), CBS, MTR, MAO-A/B, GAD, and several other extremely important ones can reduce the body’s ability to metabolize and regulate B6-dependent pathways.
These individuals may experience functional B6 overload at doses well below the toxicity thresholds seen in healthy controls.
Why Blood Levels of B6 Can Be Misleading
Why High Vitamin B6 on Blood Tests Can Misguide
When symptoms arise, many practitioners order serum or plasma B6 testing—often measured as pyridoxal-5'-phosphate (PLP). And quite often, the results come back high.
But instead of raising concern, these results are frequently dismissed as “expected” in anyone taking B6. Some doctors may even reassure the patient that their symptoms aren’t from B6, because the level isn’t “toxic.”
This is a fundamental misunderstanding of B6 metabolism.
B6 blood test results—especially plasma PLP—do not reliably reflect intracellular function or toxicity risk. It reflects what is circulating—not what is being used. In fact, high plasma B6 is frequently (but not always) a marker of poor cellular uptake. In the presence of subclinical enzymatic or transporter dysfunction, B6 can accumulate in plasma precisely because it is not entering the cells where it is needed.
This creates what could be called paradoxical B6 deficiency—a state in which someone has elevated B6 in the blood and yet still exhibits the exact signs of B6 dysfunction.
Why “Active B6” (P5P or PLP) Can Make It Worse
HOWEVER—and this is extremely important—this does not mean that the solution is to start taking “active B6” to “get the B6 into the cells”—as is the common inclination of many, many, many alternative medicine providers when plasma B6 is high.
Your high plasma B6 does not mean that you are in need of P5P—regardless of whether taking it makes you feel better or worse symptomatically (and that’s often briefly).
Again, this is sometimes (not always) a matter of faulty uptake, which is driven by a complex intersection of multiple nutrients and biochemical pathways.
P5P won’t fix that problem, and—in fact—usually will make it worse.
Functional B6 Overload: When “Too Much Function” Causes Harm
It’s not just that B6 blocks enzymes when it builds up. In many cases, it does the opposite—it ramps up the system too hard.
This is an important distinction. B6 is enzymatically active. That means when it accumulates—especially in its coenzyme form—it accelerates hundreds of reactions.
If you’re already dealing with metabolic congestion, neurotransmitter imbalance, or oxidative stress, then adding more B6 can worsen such biochemical disturbances.
In this state:
Glutamate may be converted too aggressively from glutamine or alpha-ketoglutarate, worsening excitotoxicity.
Homocysteine may be shunted excessively into the transsulfuration pathway, flooding the system with H2S and/or sulfite—especially if your CBS, SUOX, or BHMT pathways are already under- or over-performing.
GABA conversion may paradoxically stall if glutamate pools faster than GAD can buffer, or if the downstream transaminase step is slowed by low B2, iron, or magnesium.
And when these reactions overshoot, or when their products cannot be cleared or buffered fast enough, the result is systemic biochemical derangement.
This is not “toxicity” in the classic sense. Rather, it is overload—functionally almost identical to “short circuiting” your electronics.
Functional B6 toxicity, as seen here, can lead to glutamate buildup, transsulfuration overload, and symptoms that mimic other chronic illnesses.
Subtle Signs of B6 Overload Before It Becomes Toxicity
By the time you feel burning in your feet, the system is already in distress. But there can be—in some cases—earlier signs of B6 overload that often are misattributed.
Consider:
Sudden onset of vivid dreams or intense nightmares (often mistaken for “good sleep” at first)
Paradoxical anxiety from calming supplements
New facial tension, twitching, or jaw clenching
Feeling “revved up” or slightly overstimulated after meals or supplements
Loss of balance or coordination in the dark (early proprioception loss)
Increased reactivity to sulfur-containing foods or supplements
Feeling temporarily better on taurine, glycine, or molybdenum
None of these are definitive. But together, they may point toward a subclinical derailment of B6-sensitive systems—especially when paired with high plasma levels.
Differential Diagnosis: What Else Looks Like B6 Toxicity?
Conditions Often Misdiagnosed Instead of B6 Toxicity
Because symptoms of B6 overload are neurologically and metabolically diverse, they’re often mistaken for other conditions. Clinicians often mistake B6 toxicity for simple small fiber neuropathy or anxiety disorders, especially when testing only reveals high B6 without context.
Clinically, cases are often originally diagnosed as:
Small fiber neuropathy
Early autonomic neuropathy (e.g., HR variability issues, orthostatic intolerance)
MCAS (mast cell activation)
Anxiety or panic disorder
Histamine intolerance
Early MS or Parkinsonism
Chronic Lyme or mold toxicity
Perimenopausal dysautonomia
Fibromyalgia
ALS (in very rare, extreme cases)
The distinguishing feature in true B6 overload is that biochemical derangement secondary to B6 sits at the heart. That, of course, is somewhat circular. In other words, there is no one test that can definitely prove that the reason for your symptoms is B6 overload.
Importantly, even elevated plasma B6 is absolutely not a certain indicator that B6 overload is the cause of your symptoms (this is an incredibly common mistake).
Rather, this decision has to be made based on a complex consideration of lab values, symptoms, the order of symptom onset, the elimination of other possible factors, etc. And yes, the more information, the better.
Why Some People Remain in a B6 Toxic State for Years, or Even Decades
Why B6 Toxicity Symptoms Don’t Go Away After You Stop Taking It
Once symptoms start, many people stop their B6 supplements and expect things to improve quickly. But that’s not what usually happens.
Instead, they find that the tingling, buzzing, overstimulation, insomnia, or hypersensitivity either lingers for months or even worsens temporarily. This is not mysterious if you understand how B6 is handled metabolically.
Again, B6 has a long biological half-life, meaning it remains in tissues far longer than most people realize. In some cases, this means it can take sometimes months for levels to normalize—especially if tissue accumulation was high and the body's metabolic systems are strained or genetically compromised.
Even more, B6 levels in cells often remain high for long after plasma levels completely return to normal.
Receptor, Cofactors, and Mitochondrial Recovery Takes Time
But waiting it out is not the optimal approach, often because:
Downstream imbalances persist: If B6 overload triggered sulfur bottlenecks, neurotransmitter flooding, or cofactor depletion, those changes don’t instantly reverse when the B6 is stopped.
Cofactor depletion remains: Magnesium, riboflavin, zinc, etc., etc. levels may have dropped substantially during the B6-driven metabolic acceleration.
Receptor hypersensitization: Chronic overproduction of excitatory molecules like glutamate can cause sensitization of NMDA receptors, leaving the nervous system hyper-reactive for a long time afterward.
Mitochondrial strain in DRG neurons: Once energy production is compromised in sensory nerves, full recovery requires not only stopping B6 but supporting regeneration at the mitochondrial level.
In other words, once you've moved into B6 overload, removal is not enough for optimal recovery. You have to support the body’s ability to recover from the damage, correct the imbalances that have emerged, and stabilize the pathways that have been pushed off-course.
This is not a pseudoscientific judgement. I have seen this clinically. This is why “B6 detox” protocols often fail and why recovery from long-term B6 damage depends on correcting deeper biochemical imbalances.
Why Some People Feel Better on B6, Even When It’s Hurting Them
Why B6 Helps at First, Then Starts Hurting You - Short-Term Gains in Serotonin, Sulfur, or Dopamine Aren’t Always Good
Paradoxically, many people initially feel better when they start B6, even in the exact same dose that later triggers severe symptoms.
This is one of the most deceptive patterns in medicine.
This often happens because:
B6 temporarily boosts serotonin, GABA, and dopamine synthesis, creating an initial improvement in mood, calmness, or energy.
It accelerates transsulfuration, which can lower homocysteine, improve methylation flow, or reduce histamine levels, at least temporarily.
It increases glutamate-to-GABA conversion (via GAD), which may temporarily reduce neuroexcitation.
But this improvement is not sustainable. These are short-term improvements that often lead to long-term depletion, overload, or instability, via the mechanisms we discussed.
If the enzymes involved begin to stall (due to cofactor depletion or substrate exhaustion), or if intermediate products build up (like sulfite, quinolinic acid, aldehyde catecholamine intermediates, etc.), then the same B6 dose that once “helped” will now derail neurotransmission, sulfur balance, and sensory stability.
What Actually Fixes B6 Toxicity?
What to Avoid: Detoxes, P5P / PLP, and Partial Dose Reductions
There is no one-size-fits-all answer. But the answer is almost never:
Switching to P5P,
Taking a lower dose instead of stopping,
Detoxing more aggressively,
Simply waiting it out.
These may all worsen or prolong the reaction.
The Essential Recovery Pillars
Instead, the following are often essential to recovery (depending on context):
Full cessation of all B6 sources, including hidden ones in multivitamins, protein powders, hydration powders/packets, and “stress support” and “sleep support” supplements.
Support of downstream cofactors—which always must be highly personalized in dosage, form, timing, etc. I will not be recommending any specific dosages here because that’s just plain wrong (i.e. don’t got pick up 50 mg P5P tablets or 15 mg methylfolate and think that’s going to help. It’s not).
Stabilization of sulfur metabolism, especially if there are CBS, SUOX, or BHMT variants. This often involves:
Low-sulfur or modified sulfur diets short term
Targeted enzyme cofactors
Electrolyte balance
Etc.
Targeted mitochondrial support for the sensory nerves, again: purely based on your individual needs, not a generic protocol. Sometimes things like the following can help, but—again—only in the right dosage, timing, formulation, etc.
B2, B3 (in the right form), and B5
CoQ10/ubiquinol
Alpha-lipoic acid (with caution, if tolerated)
Acetyl-L-carnitine (only if it improves symptoms—can worsen in excitotoxicity)
Addressing latent imbalances in methylation, neurotransmitter recycling, or copper/zinc dynamics after the acute B6 state has stabilized.
In most cases, the best treatment for B6 overdose begins with full cessation, but true recovery requires deeper work to fix the biochemical disruption caused by functional B6 toxicity.
If you want to work with me personally: let’s talk.
Read my other articles in my new series on B6 toxicity:
B6 Toxicity Without Supplements: What It Means and Why It Happens — MTHFRSolve
Why Vitamin B6 Toxicity Can Happen at Just 2 mg Per Day — MTHFRSolve
When Prenatal B6 Backfires: How Morning Sickness Supplements Can Paradoxically Make You More Tired — MTHFRSolve
The Full List of Vitamin B6 Toxicity Symptoms (Even Without Supplements) — MTHFRSolve
Keep in mind that this is not official medical advice. No doctor-patient relationship is established through this article or through any other information provided on this website.











Slow COMT function affects how the brain and body clear dopamine, norepinephrine, and estrogen—contributing to anxiety, fatigue, supplement intolerance, and poor sleep. This guide explains the full range of symptoms, why they’re often missed, and what works to stabilize those biochemical pathways.